In conversation with US Navy Nurse Corps Captain Pamela Kilmartin, CRNA, MSNA, APRN
Drawing on her dynamic 25+ year career as a Certified Registered Nurse Anesthetist (CRNA) in the US Navy Nurse Corps and US Naval Reserve, Captain Pamela E. Kilmartin recently shared her perspectives on the realities of providing life support and anesthesia in austere and highly challenging environments.
Meet Pamela Kilmartin, CRNA, APRN CAPT, NC, USN
"Hi, I’m Pamela Kilmartin serving as a Captain with the United States Navy’s Reserve Nurse Corps as a CRNA. Currently I belong to the Navy Reserve Naval Medical Forces Development Command. I teach throughout Navy Medicine multiple resuscitative medicine classes to include Trauma Nurse Core Course and Tactical Combat Casualty Care. I also currently serve on the Bureau of Medicine and Surgery Medical Executive Committee.
As a CRNA, I have served as the Bureau of Medicine and Surgery Reserve Corps as Specialty Leader for Certified Registered Nurse Anesthetists community. Prior to being a CRNA, I was Certified Emergency Room Nurse, with 8 years of service in emergency trauma and civilian critical care fixed wing flight nursing. I have been an on-site accreditation reviewer with the American Association of Nurse Anesthetists Council on Accreditation and prior Adjunct Faculty member at the Northeastern University School of Nurse Anesthesia in Boston, MA.
I have served on the TAH-20 USNS Comfort during Pacific Partnership providing humanitarian surgical services. I was mobilized to Landsthul Regional Medical Center during Operation Enduring Freedom, and to New York City in support of the COVID-19 pandemic providing critical care transport throughout NYC from various hospitals and the USNS Comfort."

Describe the factors that are shaping how US Navy, Naval Reserve, and Marine Corps teams are delivering casualty and patient care.
"We are witnessing a significant shift from land-based operational readiness to the development of maritime medical capabilities. Our US Navy, Naval Reserve, and Marine Corps teams are now providing casualty and patient care at sea under unprecedented conditions. Recent incidents, including ship collisions at sea and fires aboard vessels in port, have highlighted the unique challenges of maritime medical operations, and the importance of solutions that address the unique demands of treating, holding, and evacuating casualties in Multi-Domain Operations (MDO)/Large Scale Combat Operations (LSCO).
These remote and/or austere environments – such as on sea vessels without dedicated medical or surgical services – introduce unique difficulties in patient care."
How will anesthesia delivery need to evolve to meet these challenges?
"Medical teams providing anesthesia in austere environments face multiple obstacles, including limited or no power supply, a restricted or nonexistent O2 source, and minimal capacity to monitor or evaluate critically ill patients during surgery.
One key challenge is the extended time required to move a patient from the point of injury to surgical stabilization while at sea, which requires Prolonged Casualty Care (PCC) and the transport of injured military personnel in an environment where medical care facilities are often limited or unavailable due to restricted air access and limited supplies of clean water, electricity, and oxygen. Medical teams must also be equipped to provide PCC in these austere and remote environments. PCC includes triage, airway management, Advanced Life Support (ALS) and Advanced Trauma Life Support (ATLS), leading to the need for damage control surgeries, treatment of environmental injuries, pain management, splinting, fracture care, and burn treatment.
With the integration of the MOVES® SLC™ and MADM™ systems, many of these limitations will be significantly improved or nearly eliminated. These technologies generate oxygen and support anesthetized patients for up to six hours on battery power, offering full Intensive Care monitoring, ventilator support and anesthesia delivery. The combination of MOVES® SLC™ and MADM™ allows for PCC and the option to establish standard surgical environments at various locations, enabling medical teams to deliver anesthesia and stabilize and monitor multiple patients until they can be transported to a higher level of care."

"The small size and ability to physically change the location of the MOVES® SLC™ and MADM™ will increase the access and enable medical personnel to get closer to where critical care and or general anesthesia services will greatly improve patient outcome. It enables the use of inhalational gas even for short procedures such as General Endotracheal Anesthesia (GETA) or Laryngeal Mask Airway (LMA) that in a non-austere environment would most likely utilize a Total Intravenous Anesthesia (TIVA) or Monitored Anesthesia Care (MAC). In the non-austere environment, unlimited choices can be made because there are few restrictions in the re-supply of consumables, oxygen supply, electricity and the heavy weight of liquid IV medications. Limiting the need to carry multiple O2 tanks and decreasing the utilization of the portable oxygen generators will now allow the medical teams to carry less volume and weight which is critical with every inch and pound in the deployed setting.
There are also factors to consider regarding the need for transportation and continued replacement of the consumables in the deployed setting to enable medical teams to provide critical care, monitoring and ventilation to include general anesthesia. The MOVES® SLC™ and MADM™ will decrease the footprint and weight necessary to provide the level of care needed. The weight of the oxygen tanks alone will make a significant impact of the safety in air transportation of ventilated patients. In addition, with the planned use of GETA the weight of one bottle of 500mg Propofol that would be one patient use is almost equivalent to the size and weight of one bottle of Sevoflurane or Isoflurane. The one bottle of inhalational gas can have up to 40 hours of anesthesia for multiple patient encounters versus the one bottle of Propofol with same size and weight providing a shorter one patient anesthesia encounter. The shelf life for Propofol once opened is 6 hours and is not intended to be used for multiple patients. Propofol also must be stored between 4°C to 25°C (40°F to 77°F)."
What are some of the specific scenarios of US Navy maritime and expeditionary support where technology can help address challenges?
"The US Navy currently employs the following three types of surgical teams for maritime and expeditionary support: Expeditionary Resuscitative Surgical System (ERSS), Fleet Surgical Teams (FST), and aircraft carrier (CVN) surgical teams. Each of these teams has specific requirements, all of which are effectively addressed by the MOVES® SLC™ and MADM™ systems."
Expeditionary Resuscitative Surgical System (ERSS)
The ERSS is the most versatile of these teams, consisting of a seven-person austere resuscitative surgical unit (Role 2 Light Maneuver or R2LM). This team provides essential medical care in remote locations whether afloat, undersea, or ashore during combat or contingency operations. Given the ERSS’s operational scope, there is a logistical need for smaller, more portable equipment; reducing the need for transporting and storing oxygen is especially important in these settings. The MOVES® SLC™ and MADM™ systems are designed to meet, and even surpass, these needs by decreasing the overall weight and footprint of the equipment.
The introduction of the MOVES® SLC™ and MADM™ anesthesia systems to the ERSS will significantly enhance patient care in austere environments, allowing for the immediate provision of anesthesia closer to the point of injury in-theater. The MADM™ anesthesia system allows the ERSS team to provide long-term multi levels of sedation/anesthesia in an austere PCC environment with minimal footprint or excessive consumable supplies.
Fleet Surgical Teams (FST)
FST are composed of 18 personnel and typically rely on host ships for surgical equipment, often constrained by the fact that these ships usually have only one operating room.
The integration of the MOVES® SLC™ and MADM™ systems will allow for the establishment of potential need of increased surgical sites on ships equipped with just one surgical location. This will enable medical personnel to administer anesthesia and provide care in austere environments, increasing capacity to manage multiple critical injuries and provide PCC to multiple patients simultaneously. FSTs are normally set up on Casualty Receiving and Treatment Ships (CRTS); therefore, they travel within an Amphibious Ready Group – Marine Expeditionary Unit (ARG-MUE). Having a mobile anesthesia workstation would allow for the FST to travel to a casualty within the ARG if needed.
Aircraft Carrier (CVN) Surgical Teams
CVN surgical teams, consisting of 55 members, are responsible for providing casualty care aboard aircraft carriers. The integration of the MOVES® SLC™ and MADM™ systems would enable these large ships ― which house the most personnel ― to establish additional operating room environments if needed. This would significantly enhance the team’s ability to administer anesthesia or provide more critical care beds improving overall patient care to more patients at the same time. Conversion of additional clean environments such as the wardroom or dining area to a makeshift surgical suite would quickly allow for teams to assist
more casualties. The small footprint and ease of transportation the MOVES® SLC™ and MADM™ will assist in the ease of transitioning these nontraditional surgical or critical care environments to a much-needed space.

How do MOVES® SLC™ and MADM™ support how US Navy, Naval Reserve, and Marine Corps teams are delivering casualty and patient care?
"The next-generation technology used in MOVES® SLC™ and MADM™ is extending critical care capabilities in austere deployment environments, addressing key gaps in existing surgical and anesthesia capabilities in combat casualty care.
When used together, MOVES® SLC™ and MADM™ can decrease the use of inhalation agents, significantly reducing consumption. This increases efficiency while easing supply chain and logistical challenges. Additionally, MOVES® SLC™ and MADM™ help mitigate the issue of waste anesthesia gas and address the challenge of limited access to large amounts of compressed oxygen, especially in remote or contested areas.
Delivering atomized inhalational gas with the low flow circle rebreathing system of the MADM™, anesthesia providers currently utilizing the system have reported an increase in hours of delivered anesthesia time. The device increases the number of hours per bottle of anesthetic gas from 16 hours up to greater than 30 hours, again utilizing multiple patient encounters with a decrease in consumable product."
How should training efforts evolve to reflect the changing landscape of austere anesthesia and related technological solutions?
The ease and speed with which medical personnel can be fully trained on MOVES® SLC™ and MADM™ addresses a key challenge: chiefly, the lack of widely available opportunities for NRM personnel to serve aboard ships that are underway. This has created a significant gap in training and mindset between the bulk of Navy Reserve Medicine Sailors and the Active Component surface fleet forces that they may be called upon to support with virtually no notice. This is changing with new opportunities to train for two-week intervals on the US Carl Vincent Aircraft Carrier starting FY 25.
With that in mind, training on technologies such as MOVES® SLC™ and MADM™ could be embedded in joint training exercises with the goal of educating and exposing multiple disciplinaries along with different levels of providers and patient care personnel to the ease of the equipment set up and assembly with various transport-compatible set up and uses. Currently there are yearly training sites such as Mac Dill AFB, Joint Base Lewis McCord and Global Medic exercises at Ft McCoy. The US Navy, USMC, Air Force and Army conduct tri-service training with multiple venues to include transportation of casualties, triage, surgical suites for damage control surgery along with PCC and staging for critical care evacuation and transport.
With this approach, US Naval Reserve personnel would be better prepared to work with Navy and Marine Corps teams to optimally deploy essential anesthesia and life-saving systems in the field, enabling them to deliver improved critical care in even the most challenging circumstances.
As both warfare and combat casualty care continue to evolve, highly adaptable, portable life-support and anesthesia solutions will be vital for delivering surgical and critical care on or near the battlefront and in transport. The mobile, compact, next generation technology of MOVES® SLC™ and MADM™ together represent a significant step forward in addressing capability gaps and improving casualty survivability.
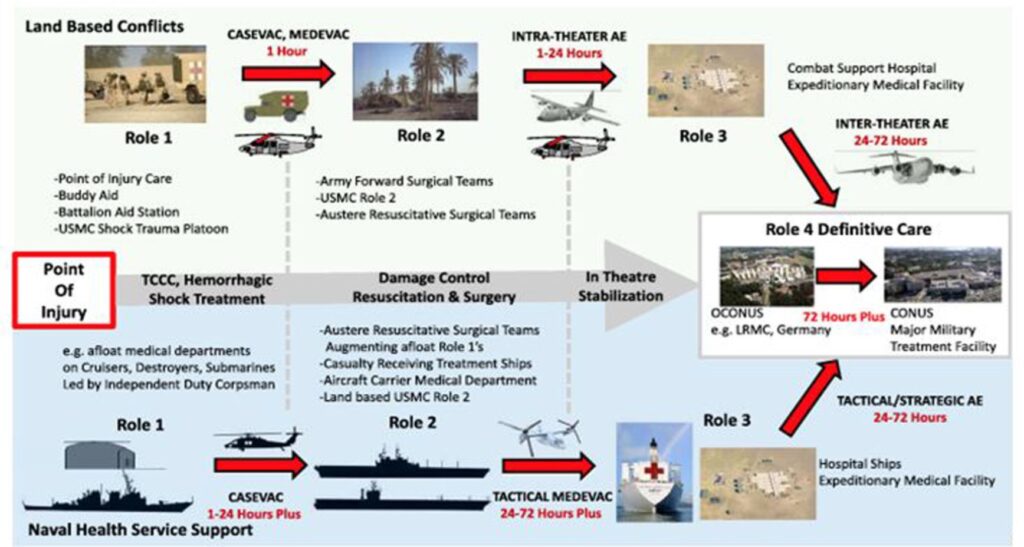
Figure 1. Maritime ERC compared to land-based roles of care progression.
Reprinted from Tadlock M, Gurney J, Tripp M, Cancio L, Sise M, Bandle J, Cubano M, Lee J, Vasquez M, Acosta J. Between the devil and the deep blue sea: a review of 25 modern naval mass casualty incidents with implications for future distributed maritime operations. J Trauma Acute Care Surg. 2021;91(2S Suppl 2):S46–S55. doi:10.1097/TA.0000000000003199.
Disclaimer: The views and opinions expressed in this article are those of the guest contributor and do not necessarily represent or reflect the views of the US Navy, US Naval Reserve or other such organizations.
